Aims and Scope: Founded in the summer of 2020, Medical hypothesis, discovery & innovation in optometry, is an international, open-access, double-blinded peer-reviewed, quarterly journal that considers publications related to optometry. The aim is to present a scientific medium of communication for researchers in the field of optometry. The journal is of interest to a broad audience of visual scientists and publishes original articles, reviews, case reports, and commentaries after a rigorous peer-review process with more interest in original articles. The journal is affiliated with and published by the "IVORC" (Registration File Number: 803630055), a registered non-profit corporation in Austin, Texas, United States. We provide English editing for papers as a complimentary free-of-charge service.
Journal Info
Impact of patching treatment on quality of life among children with amblyopia in Gaza Strip, Palestine
Medical hypothesis, discovery & innovation in optometry,
Vol. 5 No. 1 (2024),
30 April 2024
Background: Eye patching treatment affects the health-related quality of life of children with amblyopia. However, the extent of this effect in Gazan children with amblyopia remains unknown. This study evaluated the effect of patching on the health-related quality of life in Gazan children with unilateral or bilateral refractive amblyopia.
Methods: This cross-sectional study was conducted at Gaza Ophthalmic Hospital, Gaza Strip, Palestine, from September 2019 to October 2020 with adherence to the standard operating procedures of the coronavirus pandemic. Children with refractive amblyopia who completed patching therapy with a successful outcome were recruited. After patching therapy was completed, the parents completed an 18-item parental Amblyopia Treatment Index (ATI) questionnaire via telephone.
Results: Twenty-four children having 36 eyes with refractive amblyopia and a mean (standard deviation) age of 7.6 (1.8) years were included. Children underwent 2 h or 2–6 h of daily patching for 12 or 17 weeks. The mean values for total ATI score, adverse effects subscale, difficulty with compliance subscale, and social stigma subscale were 2.6, 2.6, 2.7, and 2.9, respectively, indicating that part-time patching was mostly accepted and had less impact on health-related quality of life. Treatment compliance was high; children complained at the time of patch application but did not pay attention to the patch once it was in place. In most children, the patch caused no adverse effects related to physical activities such as fun activities, learning, writing or drawing, visualizing, or playing with toys. Social stigma due to patch complications or different perceptions was not a concern. However, the perceptions of others were a major concern (n = 19, 79.2%). No significant association was found between the overall ATI score or the score of any of the subscales (adverse effects, difficulty with compliance subscale, or social stigma) and the child’s age, sex, number of lines improved in visual acuity of the amblyopic eye, severity of amblyopia, laterality, or treatment period (all P > 0.05).
Conclusions: The ATI questionnaire score and its three subscales revealed that the quality of life among Gazan children with refractive amblyopia was less affected by the part-time patching treatment. In the future, the ATI questionnaire could be used with various treatment modalities and types of amblyopia in the same setting to provide more practical guidelines on the management of amblyopia.
Contrast sensitivity assessment using the Mars letter contrast sensitivity test
Medical hypothesis, discovery & innovation in optometry,
Vol. 5 No. 1 (2024),
30 April 2024
Background: Contrast sensitivity (CS) represents an individual’s ability to detect differences in luminance between two areas and is an essential component of vision. Various studies have evaluated the relevance of different charts to assess CS in ophthalmology practice. We evaluated the CS of healthy individuals using the Mars letter CS chart.
Methods: In this hospital-based cross-sectional study, we consecutively recruited healthy individuals older than 18 years with unremarkable ocular examinations who attended the general outpatient clinic at Benue State University Teaching Hospital, Makurdi, Nigeria, between March 2021 and July 2022. Each participant was allocated to one of five groups with 10-year age intervals and 1:1 male-to-female ratios. All participants underwent a detailed ophthalmic examination. We tested visual fields using the 24-2 program on a Humphrey visual field analyzer with appropriate refractive correction. Monocular testing of CS with appropriate spectacle correction was performed using a Mars letter CS chart. The tribe, age, and sex of each individual, along with the best-corrected visual acuity (BCVA), intraocular pressure, mesopic pupil size, cup-to-disc ratio (C/D ratio), and mean deviation (MD) of the visual field for each eye were recorded.
Results: A total of 100 eyes of 50 patients with a mean (standard deviation [SD]) age of 44.6 (12.8) years and a 1:1 male-to-female ratio were enrolled. The mean (SD) CS score for the 100 included eyes was 1.67 (0.09) log units. The mean (SD) CS score was comparable between sex groups and tribes (both P > 0.05) yet differed significantly between age groups (P < 0.001). We found a significant good inverse correlation between CS score and age (r = - 0.60; P = 0.001), a low inverse correlation with BCVA (r = - 0.29; P < 0.003), and a low direct correlation with C/D ratio (r = + 0.23; P = 0.023); however, we observed no significant correlation with tribe (r = + 0.07; P = 0.053), sex (r = + 0.16; P = 0.123), IOP (r = + 0.07; P = 0.481), mesopic pupil size (r = - 0.02; P = 0.861), and mean deviation of visual field (r = + 0.02; P = 0.873).
Conclusions: We observed a progressive decline in the mean CS score in healthy eyes with each decade of increase in age. Our findings are similar to those of previous studies and could be used as reference values for the healthy population among various age groups. However, further studies with larger sample sizes are necessary to encourage clinicians to incorporate CS into routine examinations. Further studies must compare these normative values with those of disease conditions to further understand the clinical application of the CS test.
Clinical characteristics, etiologies, co-injuries, and visual outcomes of eyelid lacerations
Medical hypothesis, discovery & innovation in optometry,
Vol. 5 No. 1 (2024),
30 April 2024
Background: Eyelid trauma may be accompanied by open globe injury, canalicular injury, hyphema, angle recession, or retinal detachment. Therefore, a detailed assessment should be performed during the associated ophthalmological examinations. We assessed the demographic and clinical characteristics, etiologies, co-injuries, and visual outcomes in patients with eyelid lacerations.
Methods: This retrospective, cross-sectional study included individuals 18 years of age and older who underwent repair of an eyelid injury at our tertiary referral center between January 2021 and March 2023. Patients with known structural eyelid disorders or previous ocular surgery were excluded. Demographic and clinical data, including injury site and type, mechanism of injury, and presence of additional ocular injuries, were noted. Best-corrected visual acuity (BCVA) was recorded as the logarithm of the minimum angle of resolution (logMAR) notation at the initial and final follow-up visits.
Results: Of 195 included patients with a mean (standard deviation [SD]) age of 42.5 (5.6) years, 164 (84.1%) were men. The most common etiology was accidental (n = 70, 35.9%) and almost half of these injuries occurred at the workplace (n = 32 out of 70, 45.8%). Nine patients (4.6%) had no co-injury, 47 (24.1%) had imaging evidence of orbital bone fractures, 25 (12.8%) had nasolacrimal system involvement, and 11 (5.6%) had an open globe injury. The right upper eyelid (n = 62, 31.8%) was the most commonly affected site. Tissue loss was observed in 77 (39.5%) patients; however, no grafting was required. Five patients (2.6%) underwent lateral canthotomy to improve tissue apposition. On initial examination, 24 patients (12.3%) had traumatic myogenic ptosis, 13 (6.7%) had traumatic aponeurotic ptosis, and ptosis persisted in 7 of these 37 patients (18.9%) 6 months after laceration repair. We observed significant improvement in BCVA at the final follow-up visit (P < 0.001); at the preoperative and final visits, mean (SD) BCVA measurements were 0.21 (0.15) and 0.12 (0.07) logMAR, respectively.
Conclusions: Eyelid injuries are more common in men, and the most common etiology is accidental. These injuries occur most commonly in the workplace. Isolated eyelid lacerations are rare. Early ocular assessment and prompt management ensure better visual outcomes. We recommend preventive safety precautions for workplaces to reduce the incidence of avoidable injuries. Identifying risk factors in further population-based studies could prevent loss of labor in a productive population. Further multicenter, nationwide, longitudinal studies could estimate the actual burden and prognosis of ocular trauma, particularly that of eyelid lacerations.
Sustaining private eye care practices during initial days of the coronavirus pandemic
Medical hypothesis, discovery & innovation in optometry,
Vol. 5 No. 1 (2024),
30 April 2024
Background: The coronavirus disease 2019 (COVID-19) pandemic created new challenges for private eye care practices. Safety issues were encountered by both the healthcare workers and patients. This short communication addresses the changes made in our private eye care practice during the pandemic and the valuable lessons learned for the future.
Methods: We describe the challenges faced in our tertiary private eye care practice in India with respect to treating patients and preventing the transmission of COVID-19, considering the economic hardship within this area. We discuss the emerging economic, medical, legal, educational, and psychological issues and their solutions, which eye care hospitals could follow in the future to ensure safety without compromising quality of care.
Results: Hospitals required efficient operation with reduced fixed expenses. Clinical practices were followed in the hospital as per the recommendations of the country’s apex ophthalmic body. Proper triage and prescreening of patients at the entrance, digitalization, teleophthalmology, staggered appointments, and role-appropriate personal protective equipment were important preventive measures. The operating room protocols were modified to ensure the safety of the operating staff. Special consent was obtained from patients to safeguard against legal repercussions arising from the pandemic. The training of residents and fellows led to new avenues, including the use of digital tools. Hospitals attempted to provide counseling and psychological support to their doctors and staff during these trying times.
Conclusions: The COVID-19 pandemic will not be the last pandemic to occur in an ever-changing world. This event provided us with many new insights into the economic, clinical, legal, and psychological challenges of the COVID-19 pandemic and with ways to overcome these challenges and emerge intact. Clinical and surgical training suffered during the pandemic; however, the impact was only temporary. Clinical research gained respect because of the efforts undertaken during the pandemic. The pandemic was exceptionally harsh on many private eye care practices, and we hope to provide useful and comprehensive solutions on how to successfully navigate a similar situation if encountered in the future.
Pregnancy and diabetic retinopathy
Medical hypothesis, discovery & innovation in optometry,
Vol. 5 No. 1 (2024),
30 April 2024
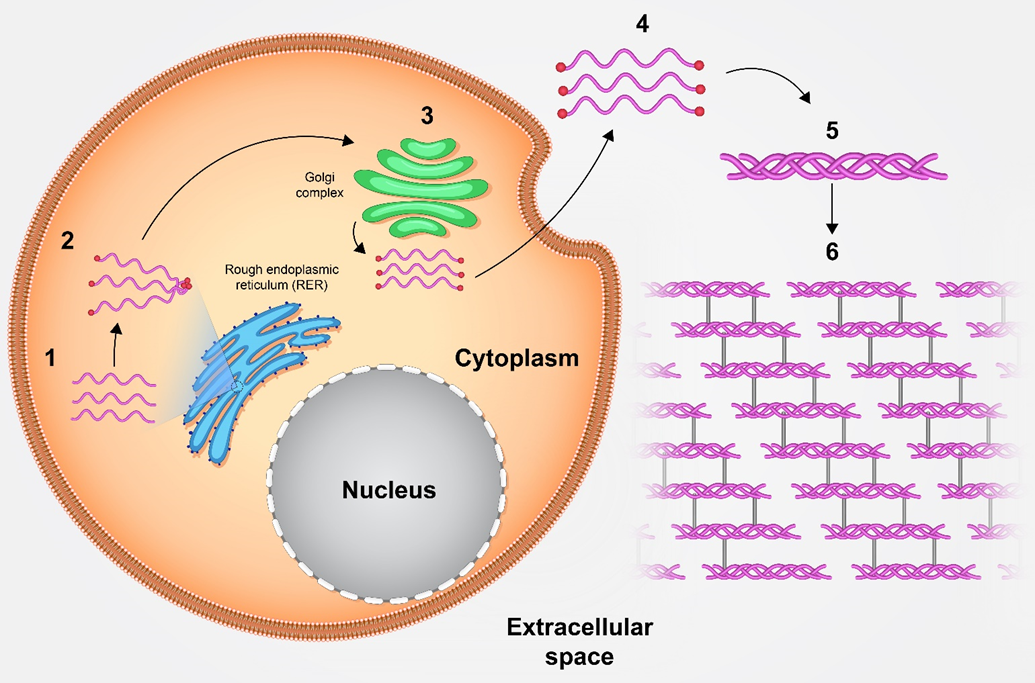
Background: An increase in the worldwide prevalence of diabetes, especially among younger populations, has led to a higher prevalence of pre-existing diabetes among pregnant women. The precise mechanisms underlying the development or progression of diabetic retinopathy (DR) during pregnancy are not entirely understood. This narrative review incorporates all available data to offer fresh insights into the pathogenesis and mechanisms of the pregnancy-induced development and/or progression of DR. Moreover, the author aims to offer clinical recommendations for DR both before conception and during pregnancy to appropriately counsel these susceptible patients.
Methods: A literature search was performed using various combinations of the following keywords: diabetes, pregnancy, diabetic retinopathy, ocular, eye, retina, microangiopathy, mechanism, pathophysiology, hyperglycemia, hypoxia, neovascularization, growth factors, immune system, blood flow, and recommendations. The search was conducted using PubMed/MEDLINE, ISI Web of Science, Scopus, and Google Scholar, and only English articles published from January 1, 2020, to December 31, 2023, involving human participants, were considered. The International Diabetes Federation Diabetes Atlas website was searched for clinical recommendations.
Results: Pregnancy-induced hyperglycemia, blood flow changes, growth factors, and the immune system play important roles in the development and progression of DR. Hyperglycemia leads to significant stress on the capillary endothelium through increased glucose flux via the polyol and hexosamine pathways, activation of protein kinase C, and increased formation of advanced glycation end-products. These pathways act in several ways that may lead to increased oxidative stress, inflammation, and vascular blockage. Thus, eye examinations are crucial before, during, and up to 12 months after pregnancy. Individuals with severe non-proliferative and proliferative DR should gradually decrease their blood glucose levels to near-normal levels over a period of 6 months before conception. Statins and medications inhibiting the renin–angiotensin system should be discontinued before pregnancy or at the initial antenatal visit if they are still being used. Retinal examinations should be performed shortly after conception and during the first trimester using tropicamide eye drops and digital imaging. Subsequent examinations should be scheduled based on DR severity at the initial examination.
Conclusions: While the precise mechanism underlying the progression of DR during pregnancy remains uncertain, the available literature suggests that pregnancy-induced hyperglycemia, blood flow changes, growth factors, and the immune system play important roles in its development and progression. Pregnant women with diabetic eye manifestations benefit from the expertise of multidisciplinary teams comprising ophthalmologists, diabetologists, and gynecologists to improve both maternal and perinatal outcomes. Moreover, postpartum follow-up requires special attention.
Slowing myopia progression in children
Medical hypothesis, discovery & innovation in optometry,
Vol. 5 No. 1 (2024),
30 April 2024
Background: A large proportion of individuals develop myopia, which is recognized as a global health concern and is predicted to increase in prevalence. Long-term eye problems are associated with myopia, particularly in young individuals. Retinal detachment and choroidal degeneration are among the causes of visual impairments associated with myopia. In this narrative review, we summarized the current measures for slowing myopia progression in children, including their safety profiles and potential drawbacks.
Methods: We conducted an English literature search for articles published between January 1, 2000, and October 31, 2023, using various combinations of keywords related to myopia, myopia progression, childhood myopia, myopia control, atropine, orthokeratology, and contact lenses. We included original or review articles pertaining to lifestyle changes and pharmacological, optical, or laser interventions for managing myopia progression in children. Our search was conducted using PubMed/MEDLINE, Google Scholar, and the Wiley Online Library. We reviewed the full text of included articles and qualitatively summarized the results of relevant studies using a narrative synthesis approach.
Results: Multiple meta-analyses indicated that increased outdoor time is associated with a lower myopia prevalence, with each extra hour spent outside each week reducing the risk of myopia by 2%. Candidate drugs, such as atropine, pirenzepine, and 7-methylxanthine, and certain intraocular pressure-lowering medications, such as timolol, have been studied in human trials for their ability to manage myopia. The nonselective antimuscarinic drug atropine, followed by the M1-selective antimuscarinic drug pirenzepine, displayed positive results in slowing myopia. Oral 7-methylxanthine, a nonselective adenosine receptor antagonist, reduces axial myopia caused by hyperopic defocus in a primate model. Low-intensity laser therapy using low doses of red and near-infrared light, visual biofeedback training, bifocal or multifocal spectacles, orthokeratology using a rigid gas-permeable contact lens, combined orthokeratology and atropine, soft contact lenses with a central distance zone and higher positive power in the periphery, and peripheral defocus contact lenses are among the interventional therapies with promising results in managing myopia progression in children.
Conclusions: The current literature supports the efficacy of increased outdoor time, administration of pharmacological agents, and special contact lenses as treatment modalities for slowing myopia progression in children. The effectiveness of orthokeratology alone and in combination with topical atropine therapy has also been assessed. Further research is needed to pinpoint the precise mechanisms of action of these therapies and to determine the best course of treatment. The increasing global prevalence of childhood myopia necessitates robust interventional studies into slowing myopia progression and preventing high myopia and related sight-threatening conditions in adulthood.